Nanobacterium Sanguineum Case Studies |
|
Case Studies from our 1st 250 Patients
#
2 MP NanobacTX for
Atherosclerosis Everywhere
#
3 FL Avoiding
Angiography in an Octogenarian
#
4 SH I'd Walk ¾’s
of a Mile for NanobacTX
#
5 CC NanobacTX for the
“Hard to Stay Open” Vessel
#
6 DM Recurrent Symptoms 15 years
out from Bypass
#
7 CW NanobacTX in Long-Standing
CV Disease
#
8 SB Refractory
Angina with Pump Dysfunction
#
9 BR Post-Bypass
Recurrent Angina
#10
BC 71% CT Score Drop in
Four Months
Cases 11-16 discuss the limitations of the Ultrafast CT scan in assessing the effectiveness of anti-Nanobacterial therapy, and explain what at first appear to be conflicting or paradoxical findings in patients with stents and prior bypass. Cases 17- 20 discuss the role of NanobacTX in several non-coronary conditions.
#11 NB: Stents Don't Decalcify - But the Rest Melts Like Butter
#12
BD: CT scores may not drop in occluded & bypassed vessels - but the patient improves nonetheless
#13 KE: The Irregular Response
#14 SJ: Measurement Error and the Threshold Effect
#16 MP: The CT Doesn't Tell the Whole Story
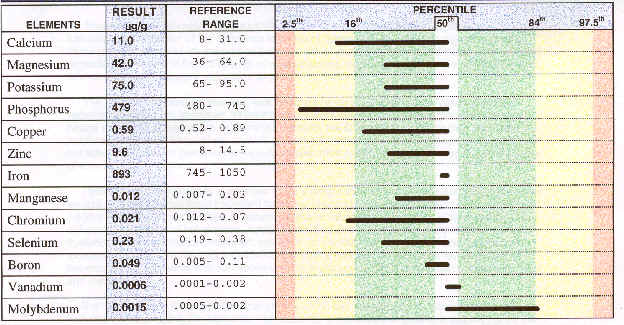
#17 LH: NanobacTX Removes Heavy Metals
#18 TM: Coronary Disease & Cardiomyopathy - Pump Dysfunction Can Improve
#21 JC: EECP and NanobacTX for single-vessel occlusive disease - watch the CRP fall
|
DATE |
EVENT |
DRUGS |
|
'85 |
Initial onset angina |
Diltiazem 120 mg |
|
‘96 |
RCA
occlusion-Inferior wall MI |
Metoprolol
200 mg |
|
10/00 |
Increased
pain-RCA 100%, LAD 80%, Circ. 60% →
4 vessel CABG |
NTG
.8mg/hr. |
|
4/01 |
Recurrent
angina; 25 episodes, 12 NTG/wk - RCA & LAD 100%, Circ. now 90%; LIMA
to LAD open and all 3 SVGs occluded |
|
|
5/01 |
EECP compromised by PVDz and PVCs → Amiodarone |
|
|
6/01 |
Arginine, Carnitine, Co-Enzyme Q10, Antioxidants, & Anodyne |
|
|
6/01 |
NanobacTX begun; baseline CT score 8,413 |
|
|
8/01 |
PVCs resolved → EECP initiated |
|
|
10/01 |
Angina minimal, NTG discontinued, & CT score 6,325 |
|
MJ was referred for EECP, but I couldn’t help him, at least not until I learned about Nanobacterium sanguineum and NanobacTX. This 52-year-old non-diabetic recent former smoker with a treated cholesterol abnormality and a 95th percentile Lp (a) presented with angina in 1985. MJ did well until ’96, when he sustained a non-extensive Right Coronary Artery (RCA) heart attack. Angiography, carried out in the fall of 2000 to evaluate increased pain, revealed 3-vessel disease, prompting 4-conduit bypass surgery. Angina returned in early 2001, and initially responded to medical therapy. Increased pain in 4/01 led to repeat angiography. The Left Anterior Descending (LAD) and Right Coronary Artery (RCA) were occluded, as expected, the Circumflex Coronary Artery (Circ) had progressed, and all three vein grafts had close down; the only inflow route left was the Left Internal Mammary Artery to Left Anterior Descending coronary artery (LIMA to LAD) bypass graft. Further surgery or catheter based intervention was not possible.
Patients with patent LIMA to LAD grafts typically do well with EECP, and MJ was referred to our program. EECP involves the inflation and deflation of segmented lower extremity pneumatic cuffs, aiming to increase diastolic coronary perfusion pressure, and by this means to encourage the recruitment and enlargement of coronary collaterals. EECP also provides a “passive exercise” effect, such that endothelial function improves and systemic nitric oxide levels rise. In patients with post-bypass 2-vessel disease, 80-90% of patients will demonstrate improved perfusion on same distance nuclear scans.
For EECP to work well, however, we need an intact lower extremity vasculature. MJ had advanced peripheral vascular disease, with 1 block claudication, compromising our ability to generate a retrograde diastolic pressure wave. For EECP to work at all, we need a stable rhythm, to allow the computer to gate cuff inflation and deflation to diastole and systole, respectively. MJ had frequent PVCs (abnormal extra heart beats), and thus we could not treat him. The only safe anti-arrhythmic agent in MJ’s case was Amiodarone, which wouldn’t begin to work for weeks to months. We began Amiodarone and waited. I kept my fingers crossed and MJ kept taking NTG tablets.
In late 5/01, I learned about N. sanguineum and NanobacTX, a combination therapy designed to reverse vascular wall calcification. At this point MJ was experiencing 25 episodes of angina each week, sometimes up to 10 episodes per day. Meds were maxed out, and arginine, antioxidants, and anodyne therapy were on board, aiming to optimize endothelial function (the endothelial cells maintain the "teflon coating" of the artery wall, and convert arginine to nitric oxide, the body's "natural nitroglycerine"). MJ’s resting EKG was markedly abnormal, demonstrating 2 mm of ST depression, just what you would see on a markedly abnormal post-treadmill stress EKG. Anti-Nanobacterial therapy made sense to me, at least while we were waiting for the Amiodarone to kick in, and MJ thus became our first NanobacTX patient. MJ’s baseline CT score was 8,413, consistent with the long-standing nature of his coronary atherosclerosis.
We were all a little apprehensive at first; weekly EKGs were obtained, to see when we could start EECP. The PVCs quieted down at four weeks, but we didn’t begin EECP, because MJ was doing a lot better. We waited another four weeks to start EECP, as EECP will work better when lower extremity blood flow is better, and MJ’s feet were warming up. Two months into NanobacTX, MJ’s angina had improved considerably, and resting ST depression had resolved. After four months of NanobacTX and two months of EECP, MJ was able to discontinue his sublingual and long-acting nitrates. MJ’s angina all but resolved, and his CT score dropped by 23%, nearly 2000 points. MJ’s C-Reactive Protein (CRP) level, an index of vascular wall inflammation, fell from 6.1 to 4.9. MJ is continuing on NanobacTX; angina remains minimal, claudication is improving, and we will repeat his CT scan in the spring.
# 2 MP: NanobacTX for Atherosclerosis Everywhere
|
DATE |
EVENT | DRUGS |
| '92 | Multivessel Bypass Surgery | Atenolol 50 mg |
| 5/01 | Class 4 angina, 1-2 episodes/day | Imdur 60 mg |
| Cath |
65%
Left Main, LAD 100% with a patent LIMA graft, RCA 100%, and all vein grafts
occluded |
|
|
Lower Ext |
Absent distal pulses; right ABI .40 and left .78 |
|
| Kidneys | Bilateral renal artery stenosis; renal cyst noted | |
| Carotids | Bilateral 50-79% narrowings; R 158/46 and L 134/49 | |
| 7/01 | Arginine, Antioxidants, Anodyne, and NanobacTX begun | |
| 9/01 | Angina minimal, left DP palpable and EECP initiated | |
| 10/01 | Angina resolved, left DP full, right ABI .71 and left .79; 50-79% carotid narrowings with R 127/40 and L 90/36 | |
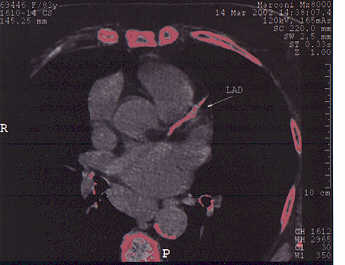
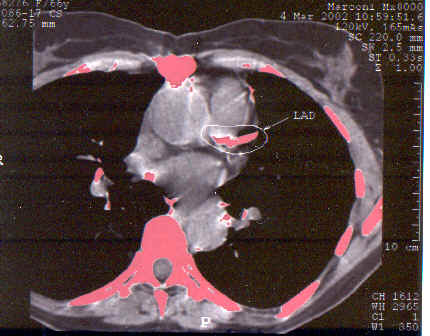
# 3 FL: Avoiding Angiography in an Octogenarian
This turned out to be a good
idea. FL tolerated four months of
NanobacTX well; angina frequency fell from 5 to 1 episode per week, NTG is no
longer required, and FL was able to increase her activity level considerably.
Her CT score fell by 26%, fibrinogen fell by 30 points, and her
cardiac-CRP value plummeted. Following an additional two months of treatment, FL's score
fell an additional 36%, so at the six month point, FL's score has fallen by
53% from baseline. A dobutamine stress echo (chemical stress echo)
demonstrated the old heart attack that we knew about, but no new abnormalities
were brought out. Subjectively and objectively FL improved. The
baseline and six month scans are shown below; with your own eye you can see the
difference in the extent of LAD calcification. FL is going to continue on NanobacTX, aiming for
complete decalcification.
|
|
Baseline |
4 months NanobacTX |
|
Fibrinogen |
430 |
400 |
|
Lp (a) |
45 |
42 |
|
CRP |
10.7 |
3.4 |
|
CT Score |
2032 |
1501 |

#4
SH: I'd Walk ¾’s
of a Mile for NanobacTX
|
DATE |
EVENT |
| '93 | Circumflex occlusion, RCA 70%, and ejection fraction 55% |
| '96 | Circumflex and RCA occlusion, marginal 70%, LAD clear and ejection fraction 20-25%; ischemia seen on Persantine cardiolite |
| '98 | EECP ® Functional class improved from 3 to 2 |
| 1/00 | Mildly abnormal 5:00 stress echo |
|
6/01 |
Abnormal
4:00 stress echo with EF falling from 40 ® 35%,
claudication at 1/4 block, and a baseline CT calcium score of 4880 |
| 7-11/01 | EECP booster, Anodyne therapy, and 4 months of NanobacTX |
| 11/01 | CT score 4034, improved 4:00 stress echo, walking 3/4 mile |
SH has battled hypertension, high cholesterol, and diabetes for years. Angiography in '93 revealed Circumflex occlusion, a small region of corresponding heart damage, a 70% RCA narrowing not amenable to angioplasty, and an ejection fraction of 55%. Three years later, a pre-operative Persantine cardiolite scan revealed ischemia and injury (insufficient blood flow and evidence of heart muscle damage) involving the heart muscle supplied by the Circumflex and RCA. Angiography demonstrated disease progression; the RCA was now occluded, and a 70% lesion had developed in a proximal branch of the Circumflex; the LAD looked good but SH’s ejection fraction (the percentage of blood cells pumped out by the heart with each beat) had fallen into the 20-25% range. Surgery wasn’t a good option here so we treated SH with EECP and got a good result.
SH returned last summer with shortness of breath with effort, his anginal equivalent, and significant claudication (effort related calf cramping, due to lower extremity vascular disease) as a new problem. He did not wish to undergo angiography, but I didn’t think that an EECP booster alone was going to get the job done, now that lower extremity blood flow was impaired. We treated SH using the MJ/MP format: four months of NanobacTX, completed with two months of EECP.
SH did well. Shortness of breath resolved, claudication is now minimal and SH can now walk 3/4ths of a mile; his CT score dropped by 17%. HS didn’t change his diet, and I didn’t change his insulin dose, but SH’s lab studies improved. Diabetic control often improves on NanobacTX; often we need to cut back on hypoglycemic therapy.
|
|
Baseline |
4 months NanobacTX |
|
FBS |
301 |
115 |
|
HbA1c |
9.7 |
7.9 |
|
HDL |
41 |
44 |
|
Triglycerides |
325 |
296 |
|
CT Score |
4880 |
4034 |
#5 CC: NanobacTX for the “hard to stay open”
vessel
#6 DM: NanobacTX 15 years out from bypass
#7
CW: NanobacTX in long-standing cardiovascular disease
|
DATE |
EVENT | DRUGS |
| '92 | Two Vessel Bypass Surgery | Atenolol 25 mg |
| '92-'98 | 10 PTCA & 4 Stent procedures | Diltiazem 180 mg |
| '98 | Metabolic intervention, Antioxidants, and L-Carnitine begun | |
| 5/01 | Claudication at 1 mall loop; max walking distance 1/2 mile - Bifemoral bruits, popliteals diminished, and distal pulses absent | |
| 6/01 | Arginine, Co-Enzyme Q10, and Anodyne therapy added | |
| 7/01 | CT score 6,426 → NanobacTX begun | |
| 10/01 | Claudication at 3 mall loops, max walking distance 1 1/2 miles - right PT diminished, left PT and DPs full; remains angina free | |
| 10/01 | 3 month CT score regressed 16% to 5,048 | |
CW underwent 2-vessel bypass surgery in ’92. 10 PTCA (angioplasty) and 4 stent procedures were needed between ’92 and ’98. In late ’98 a vein graft was stented; a 2nd lesion was non-dilatable. Metabolic intervention and a comprehensive risk factor reduction program was initiated, and to this point have kept CW out of the cath lab, and out of the hospital. Problems with lower extremity blood flow intensified last spring. CW noted claudication at one loop of the mall; maximum waking distance was ½ mile. NanobacTX was initiated, and three months later CW could complete three mall loops before claudication set in; maximum walking distance increased to 1 ½ miles. Femoral bruits resolved; right-sided distal pulses remain diminished, but popliteal and left-sided distal pulses have increased in amplitude. CW’s 3 month CT score dropped by 16%. CW is currently walking the beaches of Florida, and he is continuing to take NanobacTX.
#8
SB: NanobacTX in refractory angina with LV dysfunction
|
DATE |
EVENT |
| '88 | Five Vessel Bypass Surgery |
| 6/01 | Ejection fraction 31% with anterior wall ischemia and injury by Persantin stress cardiolite testing |
| 6/01 |
LAD,
2nd Marginal, and their SVGs occluded, ramus 80% with a
patent LIMA graft, Circumflex 30% with a patent SVG, RCA 100% with a
patent SVG, and an EF of 30%; daily angina |
| 7/01 | CT Score 2,363 ® 4 months NanobacTX and 2 months of EECP |
|
12/01 |
Angina resolved, able to walk two miles, with a CT score of 2000;- Persantin cardiolite ischemic zone decreased and EF up to 42% |
| 2/02 | 6 month CT score improved further to 1789 |
13 years out from bypass surgery, SB noted recurrent angina and shortness of breath with effort. A Persantin cardiolite study demonstrated anterior distribution ischemia and injury (insufficient blood flow and heart muscle damage involving the front wall of the heart), with a resting ejection fraction of 31%. Angiography revealed occlusion of the LAD, 2nd marginal, and their vein grafts, a patent LIMA to ramus graft, and patent vein grafts to the RCA and circumflex. SB was experiencing angina with mild activity, on average 7 times per week. EECP and NanobacTX were initiated in 7/01. Angina resolved, and SB can now walk two miles. SB’s CT calcium score fell by 18%, the ischemic zone noted on Persantin cardiolite testing decreased in size, and SB’s ejection fraction rose to 42%. Chronic ischemia leads to myocyte calcium overload. With NanobacTX we may be removing “sand” from cells as well as “pebbles” from arteries, concomitantly improving blood flow and improving impaired heart pumping function. With two additional months of NanobacTX, SB's score dropped an additional 11%. In looking at the individual arteries, you can see that the score in BS's Left Main coronary artery increased at 4 months, and then fell dramatically at 6 months, while his LAD and RCA scores fell at 4 months, and then increased slightly between 4 and 6 months. Some of this is related to measurement variability - the radiologist draws "regions of interest" over the individual arteries, and at just what point the Left Main region separates from that of the LAD is subjective. However, it is not unusual to see the score in a given artery rise before it falls. In some patients, the overall score at 4 months will be above baseline, even though their symptoms have improved. Why does this occur? We have two theories (see #15 MJ: The Up-Down Phenomena for a more detailed discussion): 1) The plaque is cracking up as opposed to dissolving, thereby occupying a greater area, and 2) We may unroofing Nanobacteria from their shelters faster than we are killing them. The unroofed Nanobacteria elaborate biofilm, attempting to create another shelter, and this biofilm lightly calcifies. Thus we are winning the battle, but at halftime it looks as if the Nanobacteria are gaining the upper hand. They may be other explanations. Regardless, the patients feel better, not worse, and if we press on the score will fall.
#9
BR: Post-Bypass Recurrent Angina
BR did well with multivessel bypass surgery in ’92. Angina recurred in ’99, associated with a mildly abnormal 9:00 stress echo study. BR did not wish to undergo angiography unless I felt it to be absolutely necessary. With a Lp (a) level at the 95th percentile at 45, I knew that BR’s restenosis risks would be increased; continued medical therapy made sense to me. Chest pain improved with an adjustment in BR’s medical regimen, but did not fully resolve. Medication cost also became an issue. With four months of anti-Nanobacterial therapy, BR’s angina improved considerably, his CT score decreased by 15%, Lp (a) fell slightly, HDL rose by 7 points, and BR’s CRP decreased from 2.0 to 0.5. BR’s hypertension improved, allowing us to drop Nifedipine 60 mg/day from BR’s regimen.
|
|
Baseline |
4 months NanobacTX |
|
Lp (a) |
45 |
38 |
|
CRP |
2.0 |
0.5 |
|
HDL |
50 |
57 |
|
CT Score |
3,240 |
2754 |
#10
BC: 71% CT Score Drop in Four
Months
To this point, our greatest numerical 4-month drop in CT score has been 2000 points; our largest percentage drop, 71%, was obtained by BC. This hypertensive, hyperlipidemic, non-diabetic, woman with a Lp (a) above 100 presented with a right hemispheric CVA in 6/01. CT described a right subcortical infarct; MRA returned normal and MRI study revealed small vessel disease with a lacunar infarct. Cardiac echo demonstrated mitral annular calcification and carotid ultrasound non-obstructive calcific plaque. Small vessel disease as opposed to embolism was felt to be the culprit. BC’s baseline coronary artery CT score was 117. Our area of interest in BC’s case is the microvasculature serving the brain; calcification in this region cannot be measured, so we used the coronary calcium burden as a surrogate marker. BC tolerated NanobacTX reasonably well, cerebrovascular symptoms have not recurred, and her coronary score dropped by 71%. Maintenance therapy and risk factor reduction will be continued.
#11 NB: Stents Don't Decalcify - But the Rest Melts Like Butter
I've read over 50 papers on the Ultrafast CT scan as a measure of coronary atherosclerosis, but in my research I have not come across any studies where the Ultrafast CT was used to evaluate patients with coronary artery stents. Stents came out five years ago as an improvement over simple coronary angioplasty. Many manufacturers have introduced many different stents, but they typically contain metal, and thus they show up on the Ultrafast CT scan - you guessed it - as calcium. Restenosis (vessel closure following angioplasty or stent placement), is less frequent following stenting as opposed to following angioplasty alone, but still occurs in 20-40% of the narrowings receiving a stent, and thus we are treating a large number of stent restenosed patients with NanobacTX and/or EECP. Now, restenosis following stent placement is not due to atherosclerosis, the N. sanguineum driven process that plugged up the artery in the first place. Rather, restenosis occurs on the basis of neointimal hyperplasia, essentially scar tissue formation (think of a kelloid scar developing in an artery), the abnormal migration of muscle cells from the muscular layer of the artery into the inner layer, plugging up the blood flow channel. While the benefits of NanobacTX in the treatment of calcific atherosclerosis are obvious, right now we really have no idea whether or not NanobacTX will prevent restenosis. We also didn't know how the presence of a stent would affect the accuracy of the Ultrafast CT as a measure of atherosclerosis. Our work with NB, and many other stented patients gave us the answer.
NB underwent LAD angioplasty and stent placement in '98. Restenosis occurred, leading to bypass surgery the following year. Bypass grafts were placed to NB's LAD and diagonal (a branch of the LAD) arteries. The Circumflex and RCA contained only mild narrowings and thus were not grafted. NB then began a comprehensive anti-atherosclerotic program; we covered every base that I knew of, and NB remains asymptomatic. We learned about the importance of N. sanguineum infection in the causation of atherosclerosis in the spring of '01, and NB began NanobacTX in June '01. Her baseline CT score was 2946, and after 3 months of NanobacTX fell just over 100 points to 2841 - NB was disappointed and I was troubled; all that work for just a 3% score reduction. NB was getting ready to leave the country for a four week vacation. To make sure that all was going well we carried out a stress echo study; she walked for 12:00 and no findings of ischemia (insufficient blood flow to the heart muscle) were observed. I sent NB packing, but asked her to pack NanobacTX in her suitcase, as I felt that with further treatment her CT score would fall. NB reluctantly agreed, and 3 months later we repeated her scan; it had again dropped only a measly 3%. We were disappointed by the total scan score, but felt a lot better when we looked at the situation artery by artery. Left Main coronary artery calcification had fully resolved, and the scores dropped by 65% and 57% respectively in the Circumflex and RCA. Look at the scan itself. The bright blob in the LAD, that looks like calcification to the scanner, is really NB's stent. The scanner can't tell the difference between a metal stent and vascular wall calcium. It's not really just that "stents don't decalcify"; what's going on here is that the Ultrafast CT score means absolutely nothing in a stented vessel! If we repeat the scan three days in a row, we will get different values; the score can rise or it can fall and it doesn't mean a thing - it's all a scanning artifact. We excise the stented artery from our thinking and use the non-stented arteries to evaluate the patient's response.
#12
BD: CT scores may not drop in occluded or bypassed vessels
-but the patient improves nonetheless
|
DATE |
EVENT | DRUGS | |||||
| '91 | Anterior Wall Heart Attack | Ismo 40 mg | |||||
| '91 | Lima to LAD and SVG to RCA | Pindolol 15 mg | |||||
| 12/91 | Lateral Wall Heart Attack - Occlusion of the non-bypassed Circumflex | ||||||
| '94 | Angina - SVG to RCA closed ® Angioplasty of RCA | ||||||
| 8/99 | Angina - RCA restenosed, Circumflex occluded, LIMA to LAD patent ® EECP with resolution of angina | ||||||
| 8/00 | Non-ischemic 9:15 stress echo | ||||||
| 6/01 | Angina - ischemic 10:19 stress echo ® NanobacTX | ||||||
| Time | Total | Left Main | LAD | Circ. | RCA | ||
| Start | 8180 | 0 | 5053 | 962 | 2165 | ||
| 4 mos. | 9098 | 0 | 5628 | 813 | 2657 | ||
| 6 mos. | 9016 | 0 | 5940 | 819 | 2256 | ||
| Lp (a) 63 ® 52 | HDL 48 ® 58 | ||||||
| 3/02 |
Angina resolved & feels great; non-ischemic 10:15 stress echo |
||||||
There’s more to medicine than making the numbers look right, so of course there's more to anti-Nanobacterial therapy than dropping the patient’s CT score. BD doesn’t smoke, his lipids and blood sugar have always been under good control, and he exercises, but he has a Lp (a) in the top 5% of the population and it’s given us fits. Lp (a), also known as the "ugly cholesterol" is designed by Mother Nature to be a "repair" particle, and it tries to "repair" angioplastied and stented vessels and bypass grafts, blocking them up. BD presented in ’91 with a non-extensive LAD distribution, anterior wall heart attack. Angiography demonstrated high-grade LAD and RCA narrowings and a moderate Circumflex narrowing. A LIMA graft was placed to the LAD and a vein graft to the RCA; the Circumflex was not narrowed enough to warrant placement of a bypass graft (if you graft moderately diseased vessels, blood will flow preferentially through the native vessel and the graft will close down).
BD returned 6 months later with a lateral infarct; his grafts looked good but the Circumflex had closed down (rapid disease progression is something we see in high Lp (a) patients); angioplasty was not possible. The SVG to the RCA closed down in ’94, but angioplasty of the native RCA resolved BD’s pain. Angina recurred in late ’99. The RCA had restenosed and was functionally occluded, the Circumflex remained closed; the only patent vessel was the LIMA graft to BD’s occluded LAD. EECP was carried out, aiming to promote collateral flow from the LIMA graft perfused distal LAD to the occluded Circumflex and RCA, and was successful. BD's angina resolved, and a follow-up 10:19 stress echo study one year later returned non-ischemic.
Angina returned in 6/01; RCA and Circumflex distribution ischemia was observed on a 9:15 stress echo study, along with a restrictive cardiac filling abnormality, indicating that BD's heart was abnormally stiff as a consequence of it's impaired blood supply. DB lived out of town, so travel was an issue, and now that we had anti-Nanobacterial therapy to offer him, we treated BD with NanobacTX rather than a booster course of EECP. BD tolerated NanobacTX well, but his CT score rose at 4 months. DB was a little miffed with me, but we have a great relationship and he agreed to two more months of treatment. Well, DB’s score fell, but only a little, and it was still above baseline, so at first you might think that, for DB anyways, that NanobacTX didn’t work!
On the other hand, BD’s angina had fully resolved, really for the first time in years. His HDL rose 10 points, and his Lp (a) dropped by 11. The restrictive filling abnormality noted on BD’s echo resolved, treadmill time increased by 1:00, and no ischemic findings were observed, so from the non-CT scan perspective, NanobacTX worked.
How can we explain this discrepancy, this mismatch between the CT findings and the patient’s clinical, laboratory, and stress test findings? It’s worth analyzing, as we often see this mismatch when treating patients with long-standing atherosclerosis and grafts.
Measurement variance can occur. In these long-standing coronary disease patients with dense calcification, it may be difficult for the radiologist to determine where calcification in the Left Main ends, and where it begins in the LAD and Circumflex. The radiologist who reads your first scan may not be the radiologist who reads your second, and the cut-off point is a little subjective, and this can lead to "shifts" in the calcium scores from one vessel to another.
The Up-Down Phenomena, to be discussed later, can occur in any patient, but peculiar to the bypassed patient are metallic artifact and the "Blind Alley" effect. Sometimes, but not always, a metal clip is used to affix the bypass graft to the bypassed artery; this will show up on the Ultrafast CT scan as calcium, the same situation as with the coronary stent - this confuses the reading.
Coronary artery calcification typically begins at the origin of a given vessel, and only slowly (over decades) extends down it's length. Our arteries also typically develop obstructive disease near their origin, often at the junction between the proximal and middle thirds. The surgeon places the bypass graft beyond the blockage (thus the term "coronary artery bypass" graft). Following surgery, blood flow runs preferentially through the open bypass graft down into the distal vessel, not through the narrowed proximal region of the vessel, so the bypassed artery typically occludes at the site of its initial narrowing. When we carry out heart catheterizations on patients with open or closed bypass grafts, we often see a "Blind Alley" phenomena. The artery is open only over it's initial 1/3rd, and thus it receives little flow. We may see that the artery is occluded in more than one location; portions may be "isolated", able to receive blood only via collateral flow. This isn't an issue clinically, as the distal vessel, which gives off the branches that actually serve the heart muscle, is getting all the oxygenated blood it needs through it's open bypass graft. However, if our goal is only to decalcify the coronary artery and make the CT scan look better, then we have a problem, as we aren't going to be able to get much NanobacTX into these blind alley or "isolated" proximal regions, the regions which typically contain the heaviest calcification. We may not, at least not within 4 months, significantly alter the natural history of calcification progression in the proximal regions (remember that coronary calcification increases at a rate of 20-80% per year). We get plenty of treatment into the distal vessels and into the microcirculation, our areas of clinical interest, but these regions don't contain much calcium, so calcium score wise, we have little to show for our work and the patient's efforts. We are certainly getting NanobacTX into the bypass grafts, but the CT scanners available today aren't able to calcium score the bypass grafts, so any improvement in graft wall calcium goes "unrecognized". Thus when we treat post-bypass patients with NanobacTX their symptoms decrease, their lab values improve, and their stress parameters increase, but the calcium scores over their bypassed vessels may not change - they may even go up, even though the patient is getting better. For these reasons, I am now typically not obtaining CT scans on my post-bypass patients. They have coronary atherosclerosis, so I know that they have a vascular wall Nanobacterial infection (bypass surgery obviously doesn't treat the patient's Nanobacterial infection - but it does buy us time), and a follow-up scan is often misleading, so why not save the patient some money, and treat them based on symptoms, stress test, and laboratory parameters, which do seem to reflect what it actually going on in the patient.
#13 KE: The Irregular Response
Patient #3 (FL: Avoiding Angiography in an Octogenarian) demonstrated gradual, uniform regression of calcification in all four of her vessels. Uniform regression of calcification makes sense intuitively, and we see this pattern in many patients, but in my practice, uniform regression is the exception rather than the rule. More often than not we we see an irregular response; such as was the case for KE.
|
DATE |
EVENT |
| 10/01 | CT score 2057 (1730 in LAD) |
|
11/01 |
10:00 stress echo with 2 mm ST depression and a LAD distribution ischemic wall motion abnormality ® NanobacTX |
|
HDL 78 ® 83 and CRP 5.8 ® 3.3 |
|
| 3/02 |
CT score 2057 ® 1834 (1730 ® 1253 in the LAD) |
KE's husband has been under my care for years; he has known coronary and cerebrovascular disease and is responding well to NanobacTX. KE herself was not experiencing cardiovascular symptoms, but she knew of the value of the Ultrafast CT as a predictor or coronary disease in asymptomatic individuals, and decided to be tested herself. This turned out to be a very good idea; KE's score was 2057, higher than that of her symptomatic husband, with a particularly high score in the LAD. A stress echo study demonstrated ischemia, an exercise revealed supply/demand mismatch in the heart muscle supplied by the LAD, consistent with the presence of a flow-limiting narrowing. We treated KE with NanobacTX over four months. She remained symptom free, as expected. Her HDL (the good cholesterol) rose by 5 points and her CRP (a key marker of vascular wall inflammation) fell nicely. A chronic, varicose vein quality, malformation on her thigh resolved (I have no explanation for this), and chronic arthritis in her knees resolved (we see this in some, but not all of our patients - NanobacTX will not resolve bone on bone arthritis but may help with joint inflammation - N. sanguineum antigen has been detected in joint fluid). Her CT score fell by 272 points, or 11%, from 2057 to 1834; her problem vessel, the LAD fell by 477 points, or 28%, while the scores over the less severely diseased Circumflex and RCA increased. How can this be? KE felt better, her lab studies looked better, her LAD score fell by 28%, and when we repeat her stress echo study (she opted for an additional four months of therapy as she wants to knock these Nanobacteria back to where they came from), it will look better. So how come the score rose in the Circumflex and RCA? Keep this thought in mind as we later discuss the limitations of the CT as a marker of disease activity and what has become to be known as the Up-Down Phenomena - our finding that the calcium score over a given artery may rise before it falls.
#14 SJ: Measurement Error and the Threshold Effect
SJ is an athletic 75 year-old who looks like a 55 year-old. He came to see me with a CT score of 13 and a request that I treat him for Nanobacterial infection. Now, in SJ's age range, a CT score of 13 is well below average, and not a score that alarmed me (but see case study #2), but SJ is planning on staying with us for another 25 years or more and he wanted to nip this problem in the bud. Also, I liked talking to SJ. He is a retired football coach, and we would discuss my sons progress (watch for Pierce Roberts at defensive end when St. Francis de Sales of Toledo wins the Ohio Division II Football Championship next year, and the year after, and the year after). SJ tolerated NanobacTX well; he remained asymptomatic and reported that weight lifting was easier for him (I remember this well, as while SJ was being treated, Pierce Roberts broke the St. Francis Freshman weight lifting record with a bench-press of 225 lbs.). So SJ, an obviously healthy man, seemed to become even healthier following anti-Nanobacterial therapy, but post-treatment his CT score rose by 146% to 38. The LAD score fell by 50%, but calcification developed in the RCA, an artery that was calcium-free at baseline - what happened here?
| Total | Left Main | LAD | Circ. | RCA | |
| Start | 13 | 0 | 13 | 0 | 0 |
| 4 mos. | 38 | 0 | 6 | 0 | 32 |
The Up-Down Phenomena, to be discussed later, may have played a role, but more likely SJ's score rose due to measurement error and the "Threshold Effect". My radiologists use a state-of-the -art Marconi Helical CT scanner; the scans are gated (the pictures are obtained at the same time within the cardiac cycle), and reproducibility is good. Cost is $350, a fair figure, and they give us a break on the follow-up scans, charging only $150. SJ had his initial and follow-up scans done on a mobile Ultrafast CT unit. These scanners are less sophisticated, may not be gated, and reproducibility is less, and that is why they cost only $100-125. Measurement artifact is going to be amplified when the baseline score is low - this may have distorted SJ's reading.
Second, a "Threshold Effect" may have occurred. The CT scanner records the density of calcium deposits in the artery wall, and reports them is units, termed Hounsfield units. The software determines a threshold, usually 130 or 90 Hounsfield units; areas of calcification with a density below this threshold value will not register on the scanner. The idea here is to minimize background clutter. If you are listening to the radio and have the volume too high, there may be a buzzing sound in the background, so you turn down the volume to eliminate the buzzing. Likewise, the scanner software ignores regions of calcification if their density is below the 130 or 90 Hounsfield unit cut-off. Our typical patient has a calcium score in the thousands, and here the "Threshold Effect" is not going to be an issue, but it may be in patients like SJ, who start out with low baseline scores. Consider a situation where there may be a region of sub-threshold calcification in one of SJ's arteries, say his RCA; it might have a calcium density of 129 units, but as it is below the cut-off of 130, it won't show up on the baseline scan. Now, if this region of calcification progresses just a little, or if measurement variance (the scanner can't be precise down to a single unit) assigns to this region a score of 130, then it will show up on the second scan, as an area of new calcification. It looks as if the patient is worse in a wholesale way, but what is really going on is that measurement variance is producing an artifact, a large percentage artifact because the baseline score is so low.
What we are going to do with SJ is to put him on maintenance therapy, involving treatment 3 consecutive days per month, and we will probably repeat his scan in two years - I doubt it will be any worse.
MJ's initial CT score response to NanobacTX scared me to death, and I imagine that it caused MJ a little concern as well.
|
DATE |
EVENT |
| 60 y/o with hypertension, an LDL of 200, prior resection of a calcified malignancy, with a CT score of 1347, on multiple nutritional supplements | |
| 8/01 | 10:00 stress echo - ST ¯ late stage 2 & apical, anterolateral, & inferior ischemic wall motion abnormalities; CT score 1347 ® NanobacTX |
| 2/02 | CT score 3070; 10:00 stress echo with slightly less ST ¯ and no ischemic wall motion abnormalities ® hold all nutritionals except Co-Enzyme Q10 and Vitamin E |
| 4/02 | CT Score 2,169; stress echo remains improved, HDL 29 ® 43 |
| 1/03 | CT Score 1209 after 14 months of treatment |
MJ felt well, he still feels well, and it will be my job to make sure that MJ feels well for another 4 to 5 decades. This health aware man in his mid-50's, with medically addressed hypertension and an elevated LDL cholesterol of 200, had a baseline CT score of 1347, evenly balanced between his Left Main, LAD, and Circumflex systems; - only his RCA was calcium-free. His stress echo study returned abnormal, just as we would expect with this degree of calcification. Years earlier, MJ had undergone surgery to remove a calcified malignancy; according to what we know about pathological calcification, N. sanguineum must have been there. MJ did not wish to undergo angiography, so we treated him with NanobacTX. MJ tolerated NanobacTX well, and he did not develop any new symptoms, so we were shocked when his 4 month CT scan came back with a score of 3070 - this wasn't measurement error; I reviewed the scans with our most experienced radiologist and it was clear that the degree of calcification had increased. Worried that I had made MJ worse, I dragged him in for a repeat stress echo study, and it looked better, not worse! I consulted with Dr. Mezo, the developer of NanobacTX, and Dr. Ciftcioglu, the world's leading authority on N. sanguineum. We put all of MJ's nutritional supplements, with the exception of Co-Enzyme Q and Vitamin E, on hold, and continued him on NanobacTX. Two months later, at the 6 month of treatment point, MJ's score dropped to 2169; his stress echo study remained improved. NanobacTX was continued, and at 8 months MJ's score was 1743. At that point an additional 500 mg of Tetracycline, taken in the morning, was added to MJ's regimen. His score rose slightly at 10 months to 1946, and then plummeted to 1209 at 14 months. NanobacTX, with the extra dose of Tetracycline will be continued, and periodically we will carry out stress echo studies and CT scans to monitor MJ's progress.
 What
happened here? A four month score increase from 1347 to 3070 is way beyond
the natural history of coronary artery calcification (20-80% progression per
year, depending on the study), so it must be a treatment related
effect. The score got worse, but MJ got better - how can we explain
this? MJ's case illustrates the phenomena of Nutritional Supplement
Interference, and serves as the most extreme example to date of the Up-Down
Effect. Soft Plaque Inertia could also have played a role (Please
Note: The following explanations are the product of my experience treating
patients, my understanding of the scientific literature, and my conversations
with the doctors at NanobacLabs and Dr. Ciftcioglu - I can't back up everything that I say in this
section with a scientific study. Within a few years, after we "get
the word out" and convince the fund-granting agencies to sponsor more
Nanobacterial research, than we will have more hard science and we will know
more. The following explanations "fit the facts" of what I see
in my patients and these explanations make sense to me).
What
happened here? A four month score increase from 1347 to 3070 is way beyond
the natural history of coronary artery calcification (20-80% progression per
year, depending on the study), so it must be a treatment related
effect. The score got worse, but MJ got better - how can we explain
this? MJ's case illustrates the phenomena of Nutritional Supplement
Interference, and serves as the most extreme example to date of the Up-Down
Effect. Soft Plaque Inertia could also have played a role (Please
Note: The following explanations are the product of my experience treating
patients, my understanding of the scientific literature, and my conversations
with the doctors at NanobacLabs and Dr. Ciftcioglu - I can't back up everything that I say in this
section with a scientific study. Within a few years, after we "get
the word out" and convince the fund-granting agencies to sponsor more
Nanobacterial research, than we will have more hard science and we will know
more. The following explanations "fit the facts" of what I see
in my patients and these explanations make sense to me).
 Now,
how, at least in theory, could we make the patients worse
with NanobacTX? How could we aggravate their vascular wall Nanobacterial
infection? Well, if we treated them with the
NanobacTX powder component and the EDTA suppository alone, without the
oral Tetracycline that is included
in the program, then we could. Recall (for a scientific discussion written
more at the MD than patient level, look in the Pathological
calcification and Nanobacterial
calcification is reversible in the Scientific Review section) that
Nanobacteria present in the vascular wall, protected from predators by their
thick calcific shelter, divide only once every 6 days. When we dissolve
their calcific shelters with EDTA and "unroof" them, the Nanobacteria
feel threatened. They responds by doubling their growth rate and
elaborating copious amounts of biofilm. The large volume of biofilm goo
which now surrounds the few Nanobacterial cell bodies begins to lightly
calcify; giving a "peanut-brittle" like appearance. If we
took a CT scan at this point, we would score calcium over a large area, even
though there are relatively few live Nanobacteria present. If we waited
for the biofilm to condense into shelters, then the area involved with
calcification would condense. If we kill the now non-sheltered and thus
vulnerable Nanobacteria with Tetracycline, than new shelters will not form
up. The Nanobacteria will be eradicated and the calcium score will drop,
eventually to zero.
Now,
how, at least in theory, could we make the patients worse
with NanobacTX? How could we aggravate their vascular wall Nanobacterial
infection? Well, if we treated them with the
NanobacTX powder component and the EDTA suppository alone, without the
oral Tetracycline that is included
in the program, then we could. Recall (for a scientific discussion written
more at the MD than patient level, look in the Pathological
calcification and Nanobacterial
calcification is reversible in the Scientific Review section) that
Nanobacteria present in the vascular wall, protected from predators by their
thick calcific shelter, divide only once every 6 days. When we dissolve
their calcific shelters with EDTA and "unroof" them, the Nanobacteria
feel threatened. They responds by doubling their growth rate and
elaborating copious amounts of biofilm. The large volume of biofilm goo
which now surrounds the few Nanobacterial cell bodies begins to lightly
calcify; giving a "peanut-brittle" like appearance. If we
took a CT scan at this point, we would score calcium over a large area, even
though there are relatively few live Nanobacteria present. If we waited
for the biofilm to condense into shelters, then the area involved with
calcification would condense. If we kill the now non-sheltered and thus
vulnerable Nanobacteria with Tetracycline, than new shelters will not form
up. The Nanobacteria will be eradicated and the calcium score will drop,
eventually to zero.
Have you ever had a skin infection? Consider acne, a boil, or cellulitis. A relatively small number of bacteria are present, microscopic in size, but as the immune system gears up to destroy them, an inflammatory response is created. The immune system first walls off the bacteria, then white blood cells enter the infected region and kill the bacteria. The area of skin surface and the volume of skin tissue involved is far grater than that of the bacterial cell bodies alone; 99% of the swelling visible on our skin as we fight off an infection is due to the immune system's inflammatory response. Now, some people have brisk inflammatory responses, while in others the degree of inflammatory swelling is less. We think that the same thing is going on in our arteries as we are unroofing and then killing Nanobacteria with NanobacTX. The unroofed Nanobacteria, if not killed instantly by Tetracycline, elaborate biofilm, enraging the immune system, to different degrees in different individuals. It may be that the immune system's inflammatory response is sequestering the Nanobacteria, perhaps making it more difficult for the Tetracycline in the blood to get to them, delaying, but not preventing their demise. The biofilm elaborated by the unroofed, under attack, Nanobacteria will begin to lightly calcify, in a loosing attempt to create a new shelter, and if we take a CT scan at that particular point, we will see an increase in the calcium score over the artery involved. It is my feeling that every region of Nanobacterial infection in every diseased artery goes through this stage of biofilm elaboration and biofilm light calcification as their long-standing vascular wall Nanobacterial infection is being eradicated. If we carried out CT scans once a week while the patient is taking NanobacTX, I predict that we would see the score over each artery (an each region within a given artery) rise and then fall. Coronary calcification is rarely evenly distributed within your arteries; this means that different arteries were infected at different times and will have different calcium scores when NanobacTX therapy is initiated. Thus each artery will demonstrate the Up-Down Phenomena at different time points. Thus, at 4 months, we may see an Irregular Response, as in patient KE, or a gross Up-Down Phenomena, as in patient MJ. We are winning the battle and the patient is getting better, and with further therapy the patients will further improve and their calcium score will eventually fall, but at half-time, judging by the CT score alone, it looks as if the Nanobacteria have the upper hand - but they don't; this is simply the UP-Down Phenomena.
On to Nutritional Supplement Interference - No patient in their right mind is going to take the NanobacTX powder and the EDTA suppository and not take the oral Tetracycline. Please note: Tetracycline is the only antibiotic that will kill Nanobacteria; Tetracycline derivatives such as Doxycycline, Terramycin, and Minocycline will not kill Nanobacteria. Tetracycline resistance is not possible; Nanobacteria are too primitive an organism to make the enzymes needed for them to become Tetracycline resistant - Dr. Ciftcioglu has never seen Tetracycline resistant Nanobacteria. It may be, however, that some patients might do better with a larger dose. 500 mg of Tetracycline, taken at bedtime along with the EDTA suppository and NanobacTX powder, is typically well-tolerated and is getting the job done, but in individuals of large stature, I may increase their dose to 1000 mg (Tetracycline can kill of beneficial gut bacteria, so I ask all of my patients to take a probiotic - cultured yogurt, Acidophilus, or a health-food store probiotic capsule - every morning to re-colonize the colon with beneficial bacteria). Many of my cardiovascular patients take Magnesium and/or Accupril. Both of these agents are of benefit to the cardiovascular patients but both Magnesium and Accupril will blunt Tetracycline absorption. It turns out that many nutritional supplements, including those that you would think contain only antioxidants or herbals, also contain magnesium. Not only will the magnesium blunt Tetracycline absorption, the magnesium, after in enters the blood stream, will be bound up by the EDTA absorbed from the rectal EDTA suppository. The EDTA-Magnesium complex will then leave the body through the kidney. The end result is that Tetracycline absorption was blunted, and you wasted one molecule of EDTA and one molecule of magnesium. There may be other components in other nutritional supplements that blunt Tetracycline absorption or interfere with the ability of the NanobacTX powder to penetrate the soft plaque and delay excretion of EDTA by the kidney - we don't have it all figured out yet but it certainly appears that certain Nutritional Supplements will Interfere with what we are trying to accomplish. We stopped MJ's nutritional supplements and his score dropped - some of this was the UP-Down Phenomena but some of the score drop was probably related to the removal of Nutritional Supplement Interference. We have now learned this lesson, and advise all NanobacTX patients to put all non-essential nutritional supplements, with the exception of Vitamin E and Co-Enzyme Q, on hold while they are taking NanobacTX (Some physician judgment is required here, as some patients, particularly those on diuretic medications, will need to be continued on mineral supplementation, particularly magnesium, but we will reduce the dose, ask the patient to take their minerals at mid-day, and we monitor them and make adjustments as needed).
Our targets, the calcified Nanobacterial shelters, are not sitting on the surface of the artery, waiting to be dissolved by the EDTA. Rather, they are imbedded in the soft plaque, kind of like chunks of fruit in a bowl of jello. To get at these nuggets of calcium, we first have to get through the soft plaque, a cholesterol-rich fatty gruel. Getting through the soft plaque is the job of the NanobacTX powder component. All of us differ in the amount of soft plaque present in our arteries, as well as the mix of soft and hard plaque present. In some patients the Nanobacterial calcific shelters may appear as grains of sand in the soft plaque goo, while in others the shelters may be larger, appearing as pebbles. Atherectomy is a revascularization procedure whereby a diamond tipped burring device is slowly advanced through an atherosclerotic narrowing, aiming to bore out a new channel. The procedure goes smoothly as the burr cuts through the soft plaque, but then it slows down when the burr comes into contact with a region of calcification (Think about drilling through a wall in you house and coming across an imbedded nail). The NanobacTX powder is also boring through the soft plaque. Our patients will of course differ in the degree of soft plaque present, and there will likely be differences between patients in the rate at which NanobacTX dissolves their soft plaque. Now, while we are laboring to get through the soft plaque, the Nanobacteria present will continue to divide once every six days, and this will show up on the patient's 4 month CT scan. Let's say you have a patient with a CT score of 200, and let's say that in this patient there is more soft plaque than is present in others, so in the first 4 months of therapy we don't get at many Nanobacterial calcific shelters. If the natural history of coronary artery calcification is progression at a rate of 40% per year, then we might expect the 4 months Ultrafast CT calcium score to be 10% greater, or 220, simply on the basis of Soft Plaque Inertia. Through in the additional concepts of Measurement Variance, the Threshold Effect, and the Up-Down Phenomenon, and you can see how the 4 month scan may not reflect what is going on in the patient. Incidentally, if we are removing soft plaque, blood flow is improving and the patient is getting better, even though the CT scan isn't yet changing in an impressive manner. Again, as a physician, I need to remember to treat the patient, not the CT scan.
#16 MP: The CT Doesn't Tell the Whole Story
We are placing a lot of emphasis on the CT scan, but as physicians, we need to remember that we are treating patients, not CT scores. This principle was reinforced to me by my experience with MP, our 16th case-study.
|
DATE |
EVENT | DRUGS |
| 8/97 | Initial onset angina | Atenolol 25 mg |
| 4/98 | 13:11 (mod protocol) stress cardiolite - inferolateral ischemia & injury ® med tnt & risk ¯ | Altace 2.5 mg |
| 11/99 | 8:00 stress echo - inferolateral ischemia and injury | |
| 11/99 | Circ 100% after 1st marginal, RCA 65%, LAD clear; EF 35 - 40% | |
| 10/01 | Recurrent symptoms - resting EF 40 - 50%; 4:53 stress echo with ST ¯, extensive inferolateral ischemia, exercise EF 40 - 50% | |
| 10/01 | CT score 2.3, all in the LAD ® NanobacTX begun | |
| 4/02 | Feels well - resting EF nl - 7:00 stress echo with ST ¯, extensive inferolateral ischemia, exercise EF increases; LDL 91 ® 67 | |
MP has well-defined coronary disease, and it's been bothering him for at least 5 years. Stress studies in '98 and '99 returned abnormal; angiography in '99 revealed Circumflex occlusion, with evidence of a prior heart attack in its distribution, and a 65% narrowing in MP's large RCA. MP did not wish to undergo RCA stenting, so we continued with medical therapy and risk factor reduction. Symptoms flared up in the fall '01. MP walked for 4:53 on the treadmill; ST depression was brought out, and a large region of heart muscle in the RCA and Circumflex distribution was seen to function poorly due to on MP's post-exercise echo images. I felt that MP was at risk for a large, 2nd heart attack, so I again brought up the issue of angiography and stent placement. MP again wished to be non-invasive, so we obtained a CT scan and began MP on NanobacTX. The surprise was MP's baseline score - only 2.3, and all of the calcium was in MP's best vessel, the LAD(more on this later). MP did beautifully with NanobacTX.
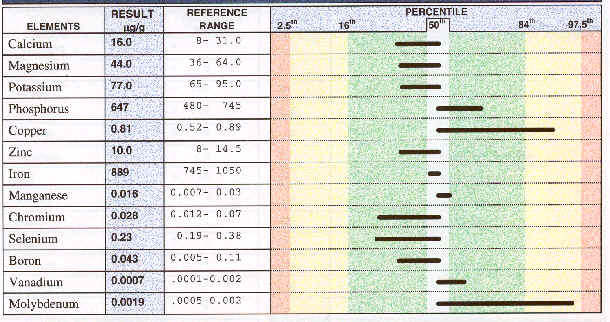
First, his LDL (bad cholesterol) plummeted, from 91 to 67. We tend to villianize cholesterol as "the cause" of heart disease, but nothing could be farther from the truth. Our body makes the stuff, so it can't be all bad. We need cholesterol to manufacture the membranes that surround our cells. We make steroid hormones, such as estrogen and testosterone, from cholesterol (think about that guys, when you take a cholesterol lowering drug and .......). It turns out that LDL cholesterol has two other jobs. First, heavy metals such as Lead, Mercury, and Cadmium, environmental toxins that play a role in heart disease, hypertension, cancer, and many other "age-related" diseases, are transported out of the body, at least in part, by LDL and other cholesterol particles. Your body may manufacture extra cholesterol, for the sole purpose of helping to rid the body of toxic metals. This maneuver has survival value; it helps protect you from heavy metal toxicity when you are young, but then you pay a price, increased susceptibility to heart disease, due to your "defensive" high cholesterol. Second, cholesterol helps buffer and neutralize bacterial endotoxin - this is material from the outer wall of pathogenic bacteria, the stuff that causes "toxic shock" and generalized inflammation when you have a serious infection. If you infect laboratory animals, there cholesterol levels will rise as a defensive response. Now, the biofilm elaborated by N. sanguineum contains an endotoxin. The NanobacTX programs kills Nanobacteria and clears them from the circulation. The EDTA provided in the NanobacTX treatment cracks a hole in the vascular wall Nanobacterial shelters, that is its primary job, but it also will remove toxic metals, transporting them from your internal organs out through the urine. So NanobacTX removes from your body two of the reasons to have a high cholesterol level. We see a rise in HDL (the good cholesterol) in nearly all patients treated with NanobacTX; frequently, but not always, we also see a reduction in LDL (the bad cholesterol) and in the total cholesterol value. Lowering cholesterol by removing its pathologic causes seems (at least to me) preferable to taking drugs that lower the cholesterol level without addressing the factors that caused it to be abnormally high in the first place. And by the way, cholesterol reduction with drugs does blunt the rate at which coronary calcification progresses, but it doesn't stabilize the calcium score, and it doesn't reverse it; the only therapy that can reverse vascular wall calcification is NanobacTX. NanobacTX works whether the cholesterol is high, low, or indifferent. Thus I no longer feel that cholesterol is "the cause" of heart disease - rather I feel that N. sanguineum infection is the primary culprit.
Second, MP's symptoms all but resolved. After 4 months of NanobacTX, ST depression and a wall motion abnormality could still be brought out, but MP's treadmill time had increased by just over 2:00. MP's resting and exercise ejection fraction (the percentage of red cells that the heart pumps out with each beat, a measure of the heart's pumping ability), both improved. MP is going to continue with NanobacTX; anticipate that his next stress test will look even better.
As a general rule, atherosclerotic plaque is 1/5th calcium, so the calcium score will reflect the extent of atherosclerotic blockage in your vessels. There are exceptions to all rules, at least in biology. A score of 2.3 in a 70 year-old like MP suggests the presence of only minor, certainly non-obstructive coronary atherosclerosis, but in MP it reflected the presence of obstructive 2-vessel disease. In my practice I have two patients with CT scores of zero; neither will let me study them angiographically, but by all other parameters (NTG-responsive chest pain, abnormal stress perfusion scans and stress echo studies) I am certain that they have obstructive coronary disease. Our highest N. sanguineum blood antigen level was obtained in one of these patients. Both responded well to NanobacTX. What's going on here?
The calcium in our arteries as measured by the Ultrafast CT scan reflects the calcium in the wall of the N. sanguineum shelters present in the walls of our arteries. Typically the shelters are large and clumped together; their mass exceeds 130 Hounsfield units and is picked up by the CT scanner. The calcium (hard plaque) thus exists as pebbles mixed in with the fatty atherosclerotic gruel (soft plaque). In some patients (this is my hypothesis - when more money is available for research, the N. sanguineum calcified shelters are smaller and more spread out, more like sand than pebbles, interspersed within the soft plaque atherosclerotic gruel. These patients have a Nanobacterial infection, they respond to NanobacTX therapy, but the CT scan misses the whole process. I guess this is why my professors taught me to treat the patient and not the diagnostic test.
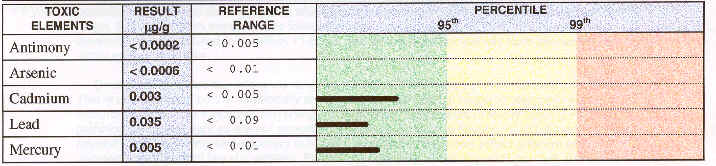
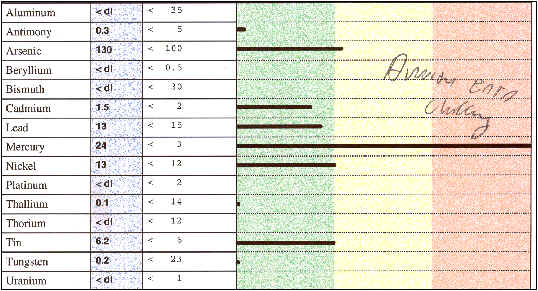
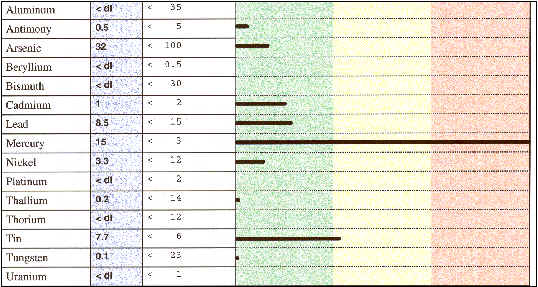
#17 LH: NANOBACTX REMOVES HEAVY METALS
| 59 y/o professor with persistent, unexplained fatigue | |
| DMPS | 24 ug Mercury/gm. creatinine ® amalgams removed |
| EDTA | Cadmium 5.1, Lead 29, and Nickel 19 ug/24 hours |
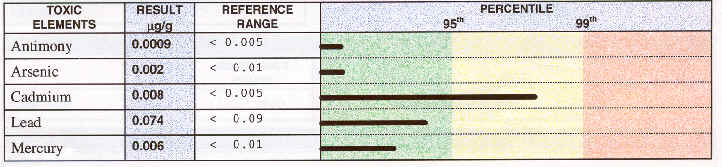
| RBC | Cadmium > 95th percentile at .008 ug/gm, Lead .074, & Mercury .006 |
| Four months NanobacTX ® significant symptomatic and laboratory improvement | |
We've been focusing on the ability of NanobacTX to eradicate vascular wall Nanobacteria, and by this means to reverse the symptoms and functional impairment in our patients with cardiovascular disease - as we should - as cardiovascular disease is our #1 killer. Nearly all of our patients have noted a significant reduction in their symptoms. We are seeing the CT scores drop in most; HDLs rise, CRPs fall, and treadmill times increase as a rule. Many patients report side-benefits, outside the realm of cardiovascular disease. Why does this occur? It may be that Nanobacterial infection was playing a role in a non-cardiovascular dysfunctional organ system, but some of these side-benefits appear to be related to the ability of the absorbed EDTA to rid the body of toxic heavy metals. Heavy metal overload is an unfortunate fact of modern day living. Our water supply may contain lead, as did automobile exhaust until recently. Arsenic is in our water, fruits and vegetables imported from the third world, and is present in treated wood products. The tobacco plant contains Cadmium, which is then deposited in the lungs of smokers. These heavy metals get into our cells, "stick" to cellular structures, displace nutritional metals such as Zinc and Magnesium, and in general gum up our metabolic works - heavy metal overload increases one's risk of cancer, heart disease, and age-related degenerative disease in general.
Can NanobacTX remove these heavy metals? If so, will patients without cardiovascular symptoms feel better following a course of treatment? LH put this concept to the test. This university professor in his mid-50's had been troubled for years by fatigue, weakness, and difficulty maintaining his concentration. He had seen doctor after doctor and undergone test after test - no real diagnosis was given. He had good days, and he had bad days when he could barely teach. On his own he learned about the problem of heavy metal overload, and how it insidiously weakens our cellular physiology to cause disease states. LH asked me to test him for heavy metal overload. First we gave LH a single dose of EDTA via the IV route; abormal amounts of Cadmium, Lead, and Nickel were observed in LH's post-EDTA 24 hour urine sample. DMPS is a heavy metal binding agent with a particular affinity for mercury; following an IV DMPS an abnormal level of Mercury was noted. LH's red cell Cadmium level was well above the 95th percentile - it was clear that LH was loaded to the gills with toxic heavy metals. So how were we going to address this situation? How were we to remove the toxic metals from LH's cells and restore his cellular biochemistry to normal?
The traditional approach would be to give LH 20-40 3,000 mg IV EDTA treatments to remove the Lead, Cadmium, and Nickel, followed by 10-15 IV DMPS treatments, focusing more on the Mercury. As 2/3rds of the Mercury burden in Americans come from their amalgam fillings (we inhale Mercury vapor with each breath if we have amalgam fillings), amalgam removal is a must.
Instead, we treated LH with a four month course of NanobacTX, our thinking being that NanobacTX provides for a lot more EDTA, but at a lower cost than when it is administered IV. LH also had his amalgam fillings removed over this four month interval. So what happened?
First of all, LH is feeling a lot better. His energy level isn't back to what it was 10 years ago, but it is a lot better than it was 10 months ago. LH can now teach, play golf, and exercise lightly without difficulty. His red blood cell Cadmium and Lead levels fell by just over 50% (not bad for 4 months work), and his post-DMPS urine Mercury level decreased from 28 to 15 (EDTA is not as efficient a Mercury binder as is DMPS, but it appears that some Mercury was removed from LH's system). The levels of some nutritional minerals also fell, also an EDTA related effect; we rectified this by adding a mineral supplement, taken at mid-day so that it will not interfere with the nighttime EDTA effect, to LH's regimen. LH's case study demonstrates that we are doing more than just killing Nanobacteria with NanobacTX - we are also removing toxic heavy metals from our patients.
#18 TM: Coronary Disease & Cardiomyopathy - Pump Dysfunction Can Improve
Patient #8 (SB: NanobacTX in Refractory Angina with Pump Dysfunction), 13 years out from bypass surgery, experienced angina relief and a CT score reduction with NanobacTX, and his ejection fraction (EF) rose by 12 points (40%), from 30 to 42%. Thus in SB's case, cardiac pumping function improved. The ejection fraction refers to the percentage of blood that the heart pumps forward with each beat. For example, if the heart fills with 100 cc of blood during its resting phase, and then ejects 50 cc of blood forward during its pumping phase, then the ejection fraction would be 50%. A normal ejection fraction is 50-55%; when a normal person runs up and down the stairs, his/her ejection fraction will rise. The lower the ejection fraction, the worse the pump dysfunction, and the worse the patient's outlook - any therapy that improves the ejection fraction is providing a significant benefit. So why did SB's EF rise? Let's look at two additional case studies and then discuss this issue:
|
DATE |
EVENT |
| TM - 59 y/o with recent onset hypertension and angina | |
| 6/01 | 3:30 ischemic stress cardiolite ® Co-Enzyme Q10 & Magnesium |
| 12/01 | EF 35-40%, generalized - worse inferolateral; mild mitral regurgitation |
| 12/01 | 10:00 stress echo - ST depression, Ventricular Tachycardia, new ischemic wall motion abnormalities; exercise EF 35-45% |
| 12/01 | NanobacTX & Atenolol 25 mg/day initiated ® angina resolved |
| 4/02 | EF 40-45% with inferolateral hypokinesis; no mitral regurgitation |
| 4/02 | 12:00 stress echo - no ST depression, no Ventricular Tachycardia; only a mild ischemic wall abnormality, with an EF of 55% |
TM first experienced angina in 6/01; a stress cardiolite scan (nuclear perfusion imaging) demonstrated impaired coronary artery blood flow; TM's treadmill time was only 3:30. TM decided against cardiac catheterization and put herself on a program of Co-Enzyme Q10, Magnesium, and other nutritional agents. I first came into contact with TM in 12/01; at that time her echo demonstrated a generalized reduction in pumping function, worse over the inferolateral wall, with an ejection fraction in the 35-40% range. My interpretation was that TM had sustained a heart attack involving the inferolateral wall of her heart, and that a 2nd process, a cardiomyopathy, was compromising pumping function elsewhere.
TM's exercise capacity had improved; she could now walk for 10:00, but her stress echo exam was markedly abnormal, with ST depression (signifying insufficient blood flow to the exercising heart muscle), Ventricular Tachycardia (an abnormal cardiac rhythm which if sustained can lead to a loss of consciousness), a new wall motion abnormality (therefore at least one additional artery had a flow limiting blockage), and only a mild rise in ejection fraction (a normal heart will respond to exercise with a rise in EF to above the normal range).
TM again did not wish to undergo cardiac catheterization, so we treated her with NanobacTX. Four months later TM was angina free. Her resting cardiac echo still revealed evidence of a prior heart attack (nothing will bring dead heart muscle back to life), but the rest of TM's heart was now functioning normally - the cardiomyopathy process had resolved. TM's ejection fraction had increased by 5 points, and the leakage across her mitral valve had resolved. Post-NanobacTX TM was able to walk 2:00 longer on the treadmill - there was no ST depression or arrhythmia and I could appreciate only a mild exercise induced wall motion abnormality; TM's exercise EF had increased to 55%. It looked like both processes, coronary artery disease and cardiomyopathy, had responded well to NanobacTX therapy.
|
DATE |
EVENT |
| GB - 79 y/o hypertensive, hyperlipidemic woman with sleep apnea | |
| 2/97 | CLBBB, 30-50% CADz, & a EF 40-45% ® Digoxin, ACE Inhibitor, Coreg, Carnitine, Co-Enzyme Q10, Antioxidants, and Lipid reduction |
| 8/00 | EF 35-40% with a restrictive filling abnormality |
| 10/01 | CT Score 2 002 ® NanobacTX begun |
| 3/02 | CT Score 1798 with a non-ischemic dobutamine stress echo; resting EF 40-50% with a reduced compliance filling pattern |
Both SB and TM had active, flow-limiting coronary disease. Heart muscle with an inadequate blood supply may not function normally. Thus some of the improvement in SB and TM's resting ejection fraction values was likely related to an improvement in coronary artery blood flow, and some was likely related to a generalized improvement in heart pumping function. GB had a more pure cardiomyopathy situation, with both "systolic" (impaired pumping function) and "diastolic" (impaired filling or "stiffness") dysfunction - her coronary arteries contained only non-flow restrictive, 30-50% narrowings, so the problem was cardiomyopathy, muscle dysfunction, alone. Pre-treatment, GB's ejection fraction was reduced at 35-40%, and her echo revealed a "restrictive" filling pattern - in other words her heart was incredibly stiff, so with exercise she would experienced shortness of breath and fatigue, despite an extensive regimen of drugs and cardiac nutritional agents.
GB's CT calcium score was 2002, consistent with her known, not flow-restrictive but still extensive coronary atherosclerosis. GB received four months of NanobacTX. With this her CT score dropped by 204 points, her ejection fraction rose into the 40-50% range, and the "restrictive" cardiac filling pattern was replaced by a less pronounced "reduced compliance" picture. Thus both systolic (pumping) and diastolic (filing) function improved with NanobacTX. A pre-operative dobutamine stress echo looked great.
Why is this occurring? Several potential explanations, none mutually exclusive, come to mind:
A) When heart muscle cells are chronically strained or over-worked, they begin to accumulate calcium. This "biochemical scaring" occurs first in the Mitochondria, the area within the cell where energy is generated. This abnormal calcium accumulation is associated with cardiac pump dysfunction, and may aggravate the situation - it may be a cause as well as an effect. Whether this intracellular calcification is Nanobacterial or metabolic in origin is a good question, but either way, the EDTA included in the NanobacTX protocol can pull it out. In the future, we should be able to calcium score the heart muscle, just as we currently score the arteries; we will probably see a reduction in abnormal heart muscle cell calcification with NanobacTX, just as we do now with arterial calcification.
B) Heavy metals can accumulate within the heart muscle cells, poisoning their biochemistry, leading to cardiomyopathy, with both systolic and diastolic dysfunction. Heavy metal cardiomyopathy in humans is probably much more common than we appreciate, and appears to be the product of exposure x a genetic susceptibility (while none of us were designed to deal with Lead, Cadmium, Mercury, and Arsenic, some of us do a better job of clearing these toxins than do others). A recent Italian study showed that cardiomyopathy patients have 20,000 times as much Mercury and Antimony in their heart muscle cells as do healthy individuals. Thus cardiomyopathy is associated with heavy metal overload. This is a scientific fact that we really shouldn't ignore - and of course we don't when we treat our patients with NanobacTX. Case study 17( LH: NanobacTX removes heavy metals) demonstrated that NanobacTX clears heavy metals from our red cells and internal organs - so with NanobacTX we have the potential to "detoxify" the cardiomyopathy patient's heart cells of heavy metals, as we concomitantly deal with muscle cell calcium overload and improve coronary artery and microvascular blood flow if they have happen to have co-existent coronary artery disease - no wonder our patients are getting better.
C) Could Nanobacterium sanguineum be a direct cause of cardiomyopathy? We don't know, but we also won't be surprised if a cause and effect relationship is eventually shown. N. sanguineum has been implicated in all calcific degenerative diseases, kidney stones, and polycystic kidney disease, so why not cardiomyopathy? We can detect N. sanguineum in the blood with the N. sanguineum antigen test - when the antigen is positive that means that uncalcified Nanobacteria were present in the blood at the time that the blood was drawn. The N. sanguineum antibody is present if uncalcified Nanobacteria have been present in the blood at some point over the last four months. Nearly all of our coronary patients have been antibody positive, and many were antigen positive as well. So far, the highest antigen levels have been found in patients with Lupus (an autoimmune disease - where the immune system attacks normal cells) and in cardiomyopathy (where immune system attack on heart muscle cells can sometimes be demonstrated). More data collection and research needs to be done here, but it just may be that N. sanguineum is playing a direct role in cardiomyopathy.
Whatever the mechanism, removal of intracellular calcium, removal of heavy metals, or direct killing of N. sanguineum in the cardiac cells, with NanobacTX it seems that patients with cardiomyopathy are getting better. If coronary insufficiency is also present, the improvement in blood flow following treatment may also be playing a role in the improved cardiac pumping function that we are see.
Under Construction
#20 BG & DE: Aortic Stenosis and Coronary Disease
Coronary artery disease is not infrequently accompanied by calcific aortic stenosis. Under normal conditions, the thin leaflets of the aortic valve open when the left ventricle, the heart's major pumping chamber, ejects oxygenated blood into the aorta, and from there on to the coronary arteries, brain, and other internal organs. In certain individuals, over the years, the aortic valve leaflets will thicken, fuse together and fibrose, and then calcify. Just why this occurs has never been explained, but this calcifying/fibrosing condition, termed aortic stenosis, is inevitably progressive. As this occurs, the left ventricle must work harder to eject a given volume of blood through the progressively narrowing aortic valve. The walls of the muscular left ventricle will thicken and stiffen (as do your arm muscles when you lift weights), initially allowing the left ventricle to compensate to this pressure overload state. As the valve narrows further, complete compensation is no longer possible; blood will begin to dam up behind the stiff, strained heart, leading to shortness of breath, initially with effort, and later at rest. Anginal chest pain can occur, even if the coronary arteries are normal, as the blood supply to the now severely thickened left ventricle cannot keep up with demand. Syncope with effort, a loss of consciousness with exercise, can develop, as the left ventricle cannot pump out enough blood to meet the needs of the brain. No medical therapy is available; aortic stenosis is a mechanical problem and it requires a mechanical solution, namely aortic valve replacement. Our approach to the patient with aortic stenosis involves watching them during the early and intermediate stages of their disease, and then deciding when the fibrosing/calcification process has progressed to the point at which valve replacement is warranted.
As the aortic valve narrows, the "pressure gradient" across the valve will increase. To eject a fixed volume of blood through the narrow valve, the left ventricle must eject it more rapidly (consider how the speed of water flow will increase as a river approaches a narrow region). To eject the blood more rapidly and overcome the impediment to ejection posed by the fibrotic, calcified aortic valve, the left ventricle must generate ever increasing pressures (in severe aortic stenosis, the left ventricular systolic pressure may be 200 mmHg, with a systolic pressure in the aorta and elsewhere of 100 mmHg - the "pressure gradient" is thus 100 mmHg). The doppler ultrasound technique allows us to measure the velocity of blood flow across the narrowed aortic valve, and from this measurement to determine peak and average pressure gradients across the valve. As the patient's aortic stenosis inevitably progresses, the pressure gradient across the valve will likewise increase. Any treatment that could open up the valve (and none has ever been proposed) would decrease the pressure gradient across the valve.
We are learning (see The Ultrafast CT Scan in the Scientific Review-NB section), that the degree of calcification in the aortic valve can be measured with the Ultrafast CT, and that the rate of progression of aortic valve calcification parallels the rate of progression of coronary calcification in a given patient. Risk factors for coronary calcification (i.e. oxidized LDL level) are also risk factors for aortic valve calcification. Statin cholesterol lowering drugs will delay progression of aortic valve calcification, parallel to their effect on the rate of coronary artery calcification in a given patient. It appears that the principles governing aortic valve calcification are the principles governing coronary artery calcification. We feel that vascular wall Nanobacterial infection is the cause of coronary artery calcification, and the case studies above have demonstrated that we can reverse coronary artery calcification with NanobacTX. The question now comes up - can we decalcify the aortic valve in our patients with aortic stenosis? Bear in mind that the narrowing in the valve is due to fibrosis as well as calcification, but in theory NanobacTX might be of value here. I do not view NanobacTX as a first line therapy for aortic stenosis, but I have treated two individuals who had moderate aortic stenosis and coronary artery disease, and their case studies are given below:
DE was troubled by shortness of breath with effort when I first saw him, and his resting echo showed calcific aortic stenosis. Doppler ultrasound demonstrated peak and average aortic valve pressure gradients of 57 and 41 mmHg respectively. His Ultrafast CT score was 546. DE walked for 9:00 on his stress test, and the post-exercise echo images were consistent with obstruction in the coronary vessels serving the back wall of DE's heart. DE did not wish to undergo catheterization or valve replacement, so we treated him with NanobacTX, aiming at his coronary arteries, and keeping our fingers crossed that it might decalcify and open up his diseased aortic valve. We do not have the technology in Toledo to measure aortic valve calcification, so our plan was to monitor the pressure gradients across DS's valve as a measure of treatment effect.
DE received 8 months of NanobacTX; with this his shortness of breath resolved and he was able to carry out moderately heavy work without difficulty. The pressure gradient across his aortic valve didn't change significantly. Post-treatment DE again walked for 9:00 on the treadmill; there was a delay in obtaining his post-exercise echo images, but echo wall motion over the back wall of DE's heart looked good, suggesting that coronary blood flow had improved. DE's CT score didn't fall, in fact it rose slightly, to 681 (we have discussed how and why the CT score can rise even when a patient has improved functionally - there may also have been some measurement error as the aortic valve calcium merges with the coronary artery calcium). DE feels well and remains physically active. My conclusion is that we improved coronary blood flow, but that we did not decalcify his arteries and that we did not open up his aortic valve with anti-Nanobacterial therapy.
|
|
Baseline | 4 months | 8 months |
| Peak gradient | 57 | 41 | 67 |
| Average gradient | 41 | not measured | 46 |
| Treadmill time | 9:00 | not done | 9:00 |
| Exercise wall motion | Abnormal - Back wall | not done | Normal |
BV has always felt well, but in 3/99 his doppler echo demonstrated peak and average aortic valve pressure gradients of 74 and 44 mmHg respectively. In 5/00 he was able to walk for 7:15 on the treadmill; the nuclear perfusion images demonstrated reduced blood flow to the side and back walls of BV's heart. BV did not want to undergo catheterization, and he began a program of IV EDTA (termed chelation therapy, the use of EDTA to remove toxic heavy metals such as Lead and Cadmium - in contrast to NanobacTX anti-nanobacterial therapy, which involves the rectal administration of EDTA, along with the NanobacTX powder component and tetracycline taken by mouth, aiming at infection of the artery wall with Nanobacterium sanguineum). A follow-up 8:00 stress echo study in 8/01 demonstrated normal cardiac wall motion, suggesting that the blood flow in BV's coronary arteries had improved, but his aortic valve pressure gradients hadn't budged.
In mid-'01, BV began a program of anti-nanobacterial therapy; he took 4 months worth of NanobacTX spaced out over 8 months. To conserve BV's out of pocket costs we did not carry out serial CT scans, and I really didn't need to carry out a follow-up stress echo study on BV, but his resting echo did show a reduction in BV's peak aortic valve pressure gradient, from 81 at baseline to 60 following treatment. We appreciate that measurement error can occur with the aortic valve pressure gradient measurement, but the change observed is certainly encouraging. BV won't let me carry out a heart catheterization on him (and he does feel great, without any significant limitations, so I'm certainly not going to push him), so our plan will be for BV to complete another 4 months of NanobacTX, again spread out over 8 months, and then to repeat the aortic valve pressure gradient measurements. We will keep our fingers crossed here.
|
|
3/99 | 8/01 - baseline | 4/01 - 4 months NanobacTX |
| Peak gradient | 74 | 81 | 60 |
| Average gradient | 44 | 43 | 44 |
#21 JC: EECP and NanobacTX for single-vessel occlusive disease - watch the CRP fall
|
DATE |
EVENT |
DRUGS |
|
'92 |
Initial onset angina - high grade RCA narrowing |
Norvasc 10 mg |
|
‘98 |
RCA
occlusion-Angioplasty not possible |
Zebeta
10 mg |
|
3/01 |
Class 4 symptoms; 4 episodes of angina/day |
Isordil
120 mg |
|
3-4/01 |
40-hour
course of EECP
→
Angina 2/day and only 3 NTGs/week needed |
|
|
5/02 |
Daily angina; 4 NTGs/week → EECP x 30 hours with heparin pre-treatment and NanobacTX begun |
|
|
8/02 |
Angina once a week and only with treadmill stress; NTG no longer required and meds decreased; CRP 5.5 → 0.9 and LDL 89 to 58 |
|
JC just couldn't form collaterals, but that's no longer a problem. JC first experienced chest pain in '92; catheterization demonstrated a high grade, non-dilatable Right Coronary Artery (RCA) narrowing. Medical therapy was initiated, aiming to decrease the oxygen demands of the heart muscle served by the RCA, and it was expected that collaterals would form from the LAD and Circ to the RCA system, and that JC's angina would ease up. Collaterals usually form in the setting of single-vessel coronary disease, but for whatever reasons, JC's vasculature could not form up a good collateral network. Enough collateral flow was present to prevent a heart attack, but not enough to resolve JC's chest pain. Repeat catheterization in '98 showed little change; the RCA had occluded, the other vessels still looked good, but collateral flow remained inadequate.
JC was referred for EECP in the spring of '01; at that time he was experiencing 4 episodes of chest pain each day, often at rest, requiring the same number of NTG tablets. Post-EECP, JC was experiencing angina only twice a day, and then only with effort. JC's NTG requirement had fallen to 3 tabs per week. JC's cholesterol panel looked good, but he had a Lipoprotein (a) of 60, well above the 95th percentile, and his CRP, our best marker of vascular wall inflammation, was similarly elevated an 5.2. A program of antioxidant vitamins, fish oil, arginine, and metabolic support was initiated and medical therapy was continued; this kept JC out of the hospital, but his Lipoprotein (a) and CRP did not budge, with values of 65 and 5.5 respectively in the spring of '02.
In the spring of '02, JC noted a slight increase in anginal frequency; some of this was because he was doing more, but his NTG requirement had increased to 4 tablets/week. A 30-hour booster session of EECP was carried out, this time with pre-EECP sublingual heparin. We typically think of heparin as a blood thinner (we give heparin IV when patients are admitted with unstable angina), but as a separate biochemical effect, heparin, if administered prior to a collateral forming stimulus, like exercise or EECP, also raises the blood level of Basic Fibroblast Growth Factor (bFGF). Like Nitric Oxide (NO) and Vascular Endothelial Growth Factor (VEGF); bFGF promotes the formation of collateral blood vessels. EECP increases NO and VEGF, and it has some effect on bFGF as well. As JC had a real problem forming collaterals, it made sense to combine two collateral forming measures, EECP and pre-EECP heparin, in our approach to JC's angina, which is really our approach to JC's collateral insufficiency. At this time we also began JC on NanobacTX.
As in the spring of '01, JC responded well to EECP; he felt the heparin augmented the EECP effect, and so did I. JC stopped EECP at 30 hours, but he continued with NanobacTX, currently at 3 1/2 months, and his improvement has continued. Angina is now occurring only once a week, and now only with treadmill exercise; NTG is no longer required. JC's LDL, previously under good control at 89, fell to 58, and his HDL rose by 3 points from 40 to 43 - we did not increase JC's Lipitor dose, this was a NanobacTX related effect. JC's Lipoprotein (a) level fell from 65 to 50, but of greater biological interest, his CRP plummeted from 5.5 to 0.9.
We know that CRP (C-Reactive Protein), our best marker of vascular wall inflammation, is also our best predictor of who will and who will not develop coronary disease, and who will have an adverse coronary event, or experience a complication or recurrence of disease following angioplasty, stent placement, or bypass surgery. Statin cholesterol lowering drugs, antioxidants, and fish oil all have been shown to lower CRP a little, but not like this. We typically see a pronounced drop in CRP when we treat cardiovascular patients with NanobacTX, and it may just be that vascular wall inflammation, due to Nanobacterium sanguineum, is the culprit underlying this ominous inflammatory marker.
Remember, the higher the CRP, the worse you are going to do, and CRP typically drops markedly with NanobacTX!